Endoscopic Retrograde cholangiopancreatography (ERCP)
Endoscopic retrograde cholangiopancreatography (ERCP) is a procedure that combines upper gastrointestinal (GI) endoscopy and x-rays to treat problems of the bile and pancreatic ducts. ERCP is also used to diagnose problems, but the availability of non-invasive tests such as magnetic resonance cholangiography has allowed ERCP to be used primarily for cases in which it is expected that treatment will be delivered during the procedure.
Upper Gastrointestinal (GI) Endoscopy
Upper GI endoscopy is a procedure that uses a lighted, flexible endoscope to see and perform procedures inside the upper GI tract. The upper GI tract includes the esophagus, stomach, and duodenum
The Bile and Pancreatic Ducts
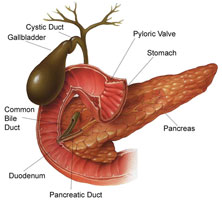
Ducts are tubelike structures in the body that carry fluids. The bile ducts carry bile, a liquid the liver makes to help break down food. A group of small bile ducts in the liver empties bile into the larger common bile duct. Between meals, the common bile duct closes and bile collects in the gallbladder.
The pancreatic ducts carry pancreatic juice, a liquid the pancreas makes to help break down food. A group of small pancreatic ducts in the pancreas empties into the main pancreatic duct. The common bile duct and the main pancreatic duct join before emptying their contents into the duodenum through the papillary orifice at the end of the duodenal papilla (a small, nipplelike structure that extends into the duodenum).
When is ERCP used?
ERCP is used when it is suspected a person’s bile or pancreatic ducts may be narrowed or blocked due to:
- tumors
- gallstones that form in the gallbladder and become stuck in the ducts
- inflammation due to trauma or illness, such as pancreatitis (inflammation of the pancreas)
- infection
- valves in the ducts, called sphincters, that won’t open properly
- scarring of the ducts, called sclerosis
- pseudocysts (accumulations of fluid and tissue debris)
How is ERCP performed?
ERCP is conducted at a hospital or outpatient center by a doctor and assistants who have specialized training in this procedure. Patients receive a local anesthetic that is gargled or sprayed on the back of the throat. The anesthetic numbs the throat and calms the gag reflex.
An intravenous needle is inserted into a vein in the arm if sedatives will be given. Doctors and other medical staff monitor vital signs while patients are sedated.
During ERCP, patients lie on their back or side on an x-ray table. The doctor inserts an endoscope down the esophagus, through the stomach, and into the duodenum. Video is transmitted from a small camera attached to the endoscope to a computer screen within the doctor’s view. Air is pumped through the endoscope to inflate the stomach and duodenum, making them easier for the doctor to examine.
When the doctor locates the duodenal papilla, a blunt tube called a catheter is slid through the endoscope and guided through the papillary opening. Once the catheter is inside the papilla, the doctor injects a dye into the ducts. The dye, also called contrast medium, allows the ducts to be seen on x-rays. X-rays are then taken to see the ducts and to look for narrowed areas or blockages.
Procedures to treat narrowed areas or blockages can be performed during ERCP. To see the ducts during treatment procedures, the doctor uses x-ray video, also called fluoroscopy. Special tools guided through the endoscope and into the ducts allow the doctor to open blocked ducts, break up or remove gallstones, remove tumors in the ducts, or insert stents. Stents are plastic or expandable metal tubes that are left in narrowed ducts to restore the flow of bile or pancreatic juice. A kind of biopsy called brush cytology allows the doctor to remove cells from inside the ducts using a brush that fits through the endoscope. The collected cells are later examined with a microscope for signs of infection or cancer.
Occasionally, ERCP is done after gallbladder surgery, if a surgical bile leak is suspected, to find and stop the leak with a temporary stent.
ERCP Risks
Significant risks associated with ERCP include
- infection
- pancreatitis
- allergic reaction to sedatives
- excessive bleeding, called hemorrhage
- puncture of the GI tract or ducts
- tissue damage from radiation exposure
- death, in rare circumstances
When ERCP is performed by an experienced doctor, complications occur in about 6 to 10 percent of patients and these often require hospitalization. Patients who experience any of the following symptoms after ERCP should contact their health care provider immediately:
- swallowing difficulties
- throat, chest, or abdominal pain that worsens
- vomiting
- bloody or dark stool
- fever
